Here’s how peelable tubing technology is leading to advances in catheterization.
Joe Rowan, Junkosha
The future of the medical tubing sector is an interesting one, not least because there are a variety of pressures on organizations within this space to provide cost-effective, highest quality products in shorter timescales. This is mainly driven by the global healthcare market, which continues to demand products and solutions that push the boundaries of what is possible at a price point that is highly competitive.
Take the catheter market as a prime example of these challenges. In the world of neurovascular techniques, clinicians are pushing for solutions that enable them to deliver complex procedures more efficiently, therefore not only reducing costs both in terms of time and money, but also enabling the provision of a higher quality of care to patients. Procedures which include delivering stents, coils and in some cases even signals/therapy down the catheter are all techniques that are moving from a “nice to have” to becoming mainstream over the next few years.
The evolution of peelable heat-shrink tubing
The peelable heat-shrink tubing (PHST) market is an exciting area to be in. Not only does it address healthcare customers’ unmet needs, but it also paves the way for progressively smaller catheter-based procedures — an ongoing requirement for medical device manufacturers.
PHST ultimately reduces total cost of ownership (TCO) for the catheter manufacturer. Since companies no longer have to use the process of skiving the heat-shrink material from the catheter, PHST can help them produce the final product more rapidly with improved yields and lower inspection levels while being more ergonomically safe.
The peelable heat shrinking process requires a very specific set of tasks, typically using a mandrel, etched PTFE liner (EPL), a sleeve of braiding, a tube of Pebax, PHST and a laminator. Having stretched the EPL liner over the mandrel and tied a knot on both ends, the catheter manufacturer should then place it into a vertical laminator, with a heating chuck on the top and a weight on the bottom enabling a consistent amount of heating and stretching. An important consideration for catheter manufacturers at this stage is the tensile strength of the EPL. In general, a high tensile strength is desirable, and many manufacturers have a proprietary process for developing that strength.
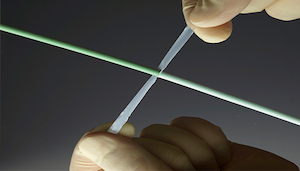
Once the first stage is completed, the etched PTFE Lined mandrel is taken out of the laminator where first the sleeve of metal braiding is placed over the liner (this delivers tortuosity to the surgeon in helping to snake the catheter around the body to get to the vessel or segment required with ease) followed by the tube of Pebax and then lastly, the PHST. The next stage is to place all of this into the laminator, where the PHST enables the reflow of all of the materials used in one continuous, robust tube. The catheter manufacturer can peel off the PHST with ease, neck the mandrel and pull it out.
Taking small to the next level
The latest innovations in PHST are based on the needs of medtech manufacturers who have asked for tubing that works on miniature guide wires used to navigate vessels that can reach a lesion or vessel segment within the brain or heart. The technology requires ultra-small PHST and high-shrink ratios. Ultra-small PHST is suitable tubing for laminating jacket coatings to tiny guidewires (e.g. 0.011 in. and 0.014 in.). PHST has shown a recovered inner diameter down to 0.009 in. A high-shrink ratio PHST (2:1) can be employed in manufacturing processes where tapered microcatheter shafts are used or where tolerance take-up is an issue.
A key benefit of PHST is that it can reduce scrap rates and decrease assembly time. Requiring only a single slit in one end to get it started, PHST peels easily along its entire length without the need for extra tools in the process, therefore saving significant time over the removal of fluorinated ethylene propylene heat-shrink tubing (FEP-HST). In addition, it enhances productivity for catheter manufacturers who can remove the PHST with ease without damaging the catheter or guide wire, therefore resulting in an ability to use the same catheter more frequently.
The move towards miniaturization and ‘active’ catheters
The trend toward miniaturization of catheters covers a wide spectrum of applications including neurovascular delivery of devices such as coils and stents for stroke or aneurysm therapies. The technology also enabled signals/energy to help support treatments such as neuromodulation or neurostimulation, such as for potential Parkinson’s disease treatments.
In addition to miniaturization, another trend for medical device makers is developing catheters that can send diagnostic signals into the body or provide therapy. These are known as “active” catheters.
Active catheters are designed to provide conduits for the delivery of signals or energy, such as for intra-vascular ultrasound. This technology is characterized by diagnostic applications such as intravenous examination of atherosclerosis, a condition in which fatty material collects along the walls of arteries, with the distal end providing signals back to data collection equipment. Therapeutic applications involve pulsed ultrasound to remove plaque, and a transcranial MRI-guided HIFU (high intensity focused ultrasound) system for the non-invasive treatment of various brain diseases such as brain cancer and Parkinson’s disease (thermal ultrasound), and stroke (mechanical ultrasound using microbubbles).
Peripheral arterial disease, where plaque builds up in arteries in the legs and in other places preventing blood flow, is usually treated using balloon angioplasty and stents. A new device, pioneered by Shockwave Medical, combines lithotripsy (sound waves to break up calcium, often used to treat kidney stones) with angioplasty balloon catheter.
Enabling catheter innovations
The miniaturization of catheters and the growing use of active catheters is challenging the medical device sector worldwide to produce solutions that enhance their use in previously inaccessible areas of the body. New tools, such as PHST, are cost-effective in reducing scrap rates whilst also increasing throughput by shortening assembly times.
Joe Rowan is Junkosha‘s president and CEO for USA and Europe. Founded in Japan in 1954, Junkosha is a pioneer of sophisticated fluoropolymer application technologies across the medical device and microwave interconnect sectors. Junkosha has three operations in Japan including its headquarters, as well as sites in the U.S., U.K. and China.
The opinions expressed in this blog post are the author’s only and do not necessarily reflect those of MedicalDesignandOutsourcing.com or its employees.